Carboplatin
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ˈkɑːrboʊˌplætən/ |
| Trade names | Paraplatin, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a695017 |
| Routes of administration | Intravenous |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | complete |
| Protein binding | Very low |
| Elimination half-life | 1.1-2 hours |
| Excretion | Kidney |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.050.388 |
| Chemical and physical data | |
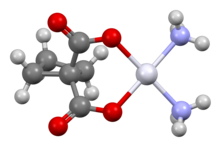
| Formula | C6H12N2O4Pt |
| Molar mass | 371.256 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Carboplatin, sold under the brand name Paraplatin among others, is a chemotherapy medication used to treat a number of forms of cancer.[3] This includes ovarian cancer, lung cancer, head and neck cancer, brain cancer, and neuroblastoma.[3] It is used by injection into a vein.[3]
Side effects generally occur.[3] Common side effects include low blood cell levels, nausea, and electrolyte problems.[4][3] Other serious side effects include allergic reactions and mutagenesis. It may be carcinogenic, but further research is needed to confirm this.[3] Use during pregnancy may result in harm to the baby.[3] Carboplatin is in the platinum-based antineoplastic family of medications and works by interfering with duplication of DNA.[3][5]
Carboplatin was developed as a less toxic analogue of cisplatin.[6] It was patented in 1972 and approved for medical use in 1989.[7] It is on the 2023 World Health Organization's List of Essential Medicines.[8]
Medical uses
[edit]Carboplatin is used to treat a number of forms of cancer. This includes ovarian cancer, lung cancer, head and neck cancer, brain cancer, and neuroblastoma. It may be used for some types of testicular cancer but cisplatin is generally more effective.[3] It has also been used to treat triple-negative breast cancer.
Side effects
[edit]Relative to cisplatin, the greatest benefit of carboplatin is its reduced side effects, particularly the elimination of nephrotoxic effects. Nausea and vomiting are less severe and more easily controlled.[9]
The main drawback of carboplatin is its myelosuppressive effect. This causes the blood cell and platelet output of bone marrow in the body to decrease quite dramatically, sometimes as low as 10% of its usual production levels. The nadir of this myelosuppression usually occurs 21–28 days after the first treatment, after which the blood cell and platelet levels in the blood begin to stabilize, often coming close to its pre-carboplatin levels. This decrease in white blood cells (neutropenia) can cause complications, and is sometimes treated with drugs like filgrastim. The most notable complication of neutropenia is increased probability of infection by opportunistic organisms, which necessitates hospital readmission and treatment with antibiotics.
Mechanism of action
[edit]Carboplatin differs from cisplatin in that it has a bidentate dicarboxylate (the ligand is cyclobutane dicarboxylate, CBDCA) in place of the two chloride ligands. Both drugs are alkylating agents. CBDCA and chloride are the leaving groups in these respective drugs Carboplatin exhibits slower aquation (replacement of CBDCA by water) and thus slower DNA binding kinetics, although it forms the same reaction products in vitro at equivalent doses with cisplatin. Unlike cisplatin, carboplatin may be susceptible to alternative mechanisms. Some results show that cisplatin and carboplatin cause different morphological changes in MCF-7 cell lines while exerting their cytotoxic behaviour.[10] The diminished reactivity limits protein-carboplatin complexes, which are excreted. The lower excretion rate of carboplatin means that more is retained in the body, and hence its effects are longer lasting (a retention half-life of 30 hours for carboplatin, compared to 1.5-3.6 hours in the case of cisplatin).
Like cisplatin, carboplatin binds to and cross-links DNA, interfering with the replication and suppressing growth of the cancer cell.[11][12]
Dose
[edit]Prior to 1989, most carboplatin dosing used body surface area dosing as with other chemotherapy. However, toxicity from treatment was variable, and therefore Professor Hillary Calvert (University of Newcastle) developed a formula to dose Carboplatin based on renal function.
Calvert's formula considers the creatinine clearance and the desired area under curve.[13] After 24 hours, close to 70% of carboplatin is excreted in the urine unchanged. This means that the dose of carboplatin must be adjusted for any impairment in kidney function.[14]
Calvert formula:
The typical area under the curve (AUC) for carboplatin ranges from 3-7 (mg/ml)*min.[14] GFR (Glomerular Filtration Rate) is a measure or estimate of kidney function. This is either measured, by measuring clearance of a radioisotope or estimated using serum and (sometimes) urine creatine measurements[15].
The Calvert formula was developed in 18 patients with GFR measurements up to 133ml/min[14]. It's applicability at very high doses of carboplatin has been challenged[16] and in the US the Food and Drug Administration has recommended capping GFR at 125ml/min[17]. This may be more important where dosing is based on calculations using more modern methods of creatinine measurement. The approach is not supported by all clinicians and certainly less so in those treating seminomas.[18]
Synthesis
[edit]Cisplatin reacts with silver nitrate and then cyclobutane-1,1-dicarboxylic acid to form carboplatin.[19]

History
[edit]Carboplatin, a cisplatin analogue, was developed by Bristol Myers Squibb and the Institute of Cancer Research in order to reduce the toxicity of cisplatin.[6][20] It gained U.S. Food and Drug Administration (FDA) approval for carboplatin, under the brand name Paraplatin, in March 1989. Starting in October 2004, generic versions of the drug became available.
Research
[edit]Carboplatin has also been used for adjuvant therapy of stage 1 seminomatous testicular cancer. Research has indicated that it is not less effective than adjuvant radiotherapy for this treatment, while having fewer side effects.[21] This has led to carboplatin based adjuvant therapy being generally preferred over adjuvant radiotherapy in clinical practice.[22]
Carboplatin combined with hexadecyl chain and polyethylene glycol appears to have increased liposolubility and PEGylation. This is useful in chemotherapy, specifically for non-small cell lung cancer.[23]
References
[edit]- ^ "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 Oct 2023.
- ^ "Product monograph brand safety updates". Health Canada. 7 July 2016. Retrieved 3 April 2024.
- ^ a b c d e f g h i "Carboplatin". The American Society of Health-System Pharmacists. Archived from the original on 21 December 2016. Retrieved 8 December 2016.
- ^ Oun R, Moussa YE, Wheate NJ (May 2018). "The side effects of platinum-based chemotherapy drugs: a review for chemists". Dalton Transactions. 47 (19): 6645–6653. doi:10.1039/c8dt00838h. PMID 29632935.
- ^ Apps MG, Choi EH, Wheate NJ (August 2015). "The state-of-play and future of platinum drugs". Endocrine-Related Cancer. 22 (4): R219–R233. doi:10.1530/ERC-15-0237. hdl:2123/24426. PMID 26113607.
- ^ a b Lebwohl D, Canetta R (1998). "Clinical development of platinum complexes in cancer therapy: an historical perspective and an update". Eur J Cancer. 34 (10): 1522–34. doi:10.1016/s0959-8049(98)00224-x. PMID 9893623.
- ^ Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 513. ISBN 9783527607495. Archived from the original on 2016-12-20.
- ^ World Health Organization (2023). The selection and use of essential medicines 2023: web annex A: World Health Organization model list of essential medicines: 23rd list (2023). Geneva: World Health Organization. hdl:10665/371090. WHO/MHP/HPS/EML/2023.02.
- ^ Gulbis AM, Wallis WD (2023). "10 - Preparative Regimens Used in Hematopoietic Cell Transplantation and Chimeric Antigen Receptor T-Cell Therapies". Manual of Hematopoietic Cell Transplantation and Cellular Therapies. Elsevier. pp. 125–143. doi:10.1016/B978-0-323-79833-4.00010-3. ISBN 9780323798334.
- ^ Natarajan G, Malathi R, Holler E (November 1999). "Increased DNA-binding activity of cis-1,1-cyclobutanedicarboxylatodiammineplatinum(II) (carboplatin) in the presence of nucleophiles and human breast cancer MCF-7 cell cytoplasmic extracts: activation theory revisited". Biochemical Pharmacology. 58 (10): 1625–1629. doi:10.1016/S0006-2952(99)00250-6. PMID 10535754.
- ^ Noll DM, Mason TM, Miller PS (February 2006). "Formation and repair of interstrand cross-links in DNA". Chemical Reviews. 106 (2): 277–301. doi:10.1021/cr040478b. PMC 2505341. PMID 16464006.
- ^ Edelman MJ, Rupard EJ (2006). "TUMORS, MALIGNANT / Chemotherapeutic Agents". Encyclopedia of Respiratory Medicine. Academic Press. pp. 332–338. doi:10.1016/B0-12-370879-6/00409-9. ISBN 9780123708793.
- ^ O'Cearbhaill R, Sabbatini PS (September 1, 2012). "New Guidelines for Carboplatin Dosing". Memorial Sloan Kettering Cancer Center. Archived from the original on 2014-10-31. Retrieved 2014-03-27.
- ^ a b c Calvert AH, Newell DR, Gumbrell LA, O'Reilly S, Burnell M, Boxall FE, et al. (November 1989). "Carboplatin dosage: prospective evaluation of a simple formula based on renal function". Journal of Clinical Oncology. 7 (11): 1748–1756. doi:10.1200/JCO.1989.7.11.1748. PMID 2681557.
- ^ Donahue A, McCune JS, Faucette S, Gillenwater HH, Kowalski RJ, Socinski MA, Lindley C (2001-05-14). "Measured versus estimated glomerular filtration rate in the Calvert equation: influence on carboplatin dosing". Cancer Chemotherapy and Pharmacology. 47 (5): 373–379. doi:10.1007/s002800000260. ISSN 0344-5704. PMID 11391850.
- ^ Mazumdar M (2000-09-06). "Calvert's Formula for Dosing Carboplatin: Overview and Concerns of Applicability in High-Dose Setting". Journal of the National Cancer Institute. 92 (17): 1434–1436. doi:10.1093/jnci/92.17.1434. PMID 10974080.
- ^ Research Cf. "About the Center for Drug Evaluation and Research - Carboplatin dosing". www.fda.gov. Archived from the original on 2017-01-18. Retrieved 2024-12-26.
- ^ Fehr M, Maranta AF, Reichegger H, Gillessen S, Cathomas R (2018). "Carboplatin dose based on actual renal function: no excess of acute haematotoxicity in adjuvant treatment in seminoma stage I". ESMO Open. 3 (3): e000320. doi:10.1136/esmoopen-2018-000320. PMC 5844370. PMID 29531843.
- ^ Vardanyan RS, Hruby VJ (2006). "30 - Antineoplastics". Synthesis of Essential Drugs. Elsevier. pp. 389–418. doi:10.1016/B978-044452166-8/50030-3. ISBN 9780444521668.
- ^ "Discovering early chemotherapy drugs". Institute of Cancer Research. Retrieved 2023-10-06.
- ^ Oliver RT, Mason MD, Mead GM, von der Maase H, Rustin GJ, Joffe JK, et al. (2005). "Radiotherapy versus single-dose carboplatin in adjuvant treatment of stage I seminoma: a randomised trial". Lancet. 366 (9482): 293–300. doi:10.1016/S0140-6736(05)66984-X. PMID 16039331. S2CID 6001898.
- ^ Toner GC (May 2015). "Testicular cancer: Optimal management of stage I seminoma in 2015". Nature Reviews. Urology. 12 (5): 249–251. doi:10.1038/nrurol.2015.85. PMID 25896179. S2CID 8072355.
- ^ Lang T, Li N, Zhang J, Li Y, Rong R, Fu Y (December 2021). "Prodrug-based nano-delivery strategy to improve the antitumor ability of carboplatin in vivo and in vitro". Drug Delivery. 28 (1): 1272–1280. doi:10.1080/10717544.2021.1938754. PMC 8238065. PMID 34176381.
Further reading
[edit]- Canetta R, Rozencweig M, Carter SK (September 1985). "Carboplatin: the clinical spectrum to date". Cancer Treatment Reviews. 12 Suppl A (Suppl A): 125–136. doi:10.1016/0305-7372(85)90027-1. PMID 3002623.
- Yang XL, Wang AH (September 1999). "Structural studies of atom-specific anticancer drugs acting on DNA". Pharmacology & Therapeutics. 83 (3): 181–215. doi:10.1016/S0163-7258(99)00020-0. PMID 10576292.

